
There is nothing mysterious or inherently dangerous about heroin. It is simply a delivery system for morphine.
 Following is a concise but comprehensive account of heroin. Reading time:
approximately twenty minutes.
Following is a concise but comprehensive account of heroin. Reading time:
approximately twenty minutes.
THE TRUTH ABOUT HEROIN AND THE MYTH OF FATAL 'HEROIN OVERDOSE'
THE SUBSTANCE IN BRIEF
No other drug attracts the degree of inaccurate and untrue commentary as does heroin. No other drug has been lied about so aggressively and for so long as heroin. The information on this page is not intended in any way, to endorse or encourage the use of heroin or any other opioid. The intention is solely to provide the truth, and by doing so, help prevent deaths and injury due to combining of central nervous system depressant drugs.
 Heroin is a semi-synthetic compound that breaks down into morphine once in the
body. Morphine is therefore the primary active metabolite of heroin. It is predominately morphine that exerts the effects that heroin is taken for,
whether that is pain relief in the medical setting or euphoric effects in the recreational setting.
Heroin is a semi-synthetic compound that breaks down into morphine once in the
body. Morphine is therefore the primary active metabolite of heroin. It is predominately morphine that exerts the effects that heroin is taken for,
whether that is pain relief in the medical setting or euphoric effects in the recreational setting.
 Morphine is the 'gold standard' analgesic (pain killer) for serious pain. It has
no maximum dose (it can be given until pain relief is achieved without regard to the size of the total dose) and no 'ceiling effect' (it does not
have a dose at which it ceases to have a therapeutic effect). It is also used to treat shortness of breath (dyspnoea) in the palliative-care setting.
Morphine is the 'gold standard' analgesic (pain killer) for serious pain. It has
no maximum dose (it can be given until pain relief is achieved without regard to the size of the total dose) and no 'ceiling effect' (it does not
have a dose at which it ceases to have a therapeutic effect). It is also used to treat shortness of breath (dyspnoea) in the palliative-care setting.
 The two major side effects of morphine are nausea and constipation
The two major side effects of morphine are nausea and constipation
 Morphine can induce a sense of well-being which is attractive for some people
Morphine can induce a sense of well-being which is attractive for some people
and most importantly:
 THERE IS NOT AND NEVER HAS BEEN ANY EVIDENCE TO SUPPORT THE
CONCEPT OF FATAL 'HEROIN OVERDOSE'. Modern clinical research (1) clearly
and unequivocally shows that substantial heroin overdose does not result in death due to 'respiratory depression' or arrest and that extremely high
doses result in low, therapeutic blood-morphine levels.
THERE IS NOT AND NEVER HAS BEEN ANY EVIDENCE TO SUPPORT THE
CONCEPT OF FATAL 'HEROIN OVERDOSE'. Modern clinical research (1) clearly
and unequivocally shows that substantial heroin overdose does not result in death due to 'respiratory depression' or arrest and that extremely high
doses result in low, therapeutic blood-morphine levels.
When opioids are involved in adverse drug-related events related to breathing, evidence clearly supports the following circumstance: people becoming heavily sedated due to combinations of drugs and not being able to breathe properly due to airway obstruction. This can lead to injury or death due to lack of oxygen. A combination of alcohol and morphine for instance, has long been known to be potentially dangerous.
IF YOU INTEND TO OR CURRENTLY TAKE OPIOIDS ON A RECREATIONAL OR MEDICINAL BASIS, THE FOLLOWING INFORMATION IS CRITICAL:
An intentional or accidental combination of opioids and other central nervous system depressant drugs such as alcohol and/or medications such as benzodiazepines, anti-depressants and anti-histamines, can give rise to a dangerous situation. Heavy sedation from a combination of different drugs can lead to a physical barrier to breathing in your throat (airway obstruction).

Representation of airway obstruction
Airway obstruction in the context of substance use is when you are unable to breathe properly due to the position of your head, jaw (and therefore structures such as the tongue) and/or the presence of vomit. This occurs because you are unconscious (heavily sedated) due to a combination of drugs and are unable to make the necessary adjustments to head and jaw position to ensure an open airway.
This situation is not unique to combinations of drugs containing opioids: it can occur due to many combinations not involving opioids.
If you wish to take opioids safely, do not mix them with other drugs or medications. If you do, you may become so heavily sedated that breathing becomes difficult or impossible due to airway obstruction.
 If you have already taken a central nervous
system depressant drug (such as alcohol or a prescribed medication), do not then take an opioid.
If you have already taken a central nervous
system depressant drug (such as alcohol or a prescribed medication), do not then take an opioid.
 If you have already taken an opioid, do
not then take another central nervous system depressant drug (such as alcohol or a prescribed medication).
If you have already taken an opioid, do
not then take another central nervous system depressant drug (such as alcohol or a prescribed medication).
If you are intent on combining drugs, do so with caution, as airway obstruction can lead to permanent disability or death.
Read about multiple-drug toxicity in the 'Overdose' page
HEROIN
A detailed and referenced account.
INTRODUCTION
The purpose of the following is to present the truth about heroin in a brief conceptual manner. The intention is not to promote the substance, but merely to counter the misinformation that is constantly disseminated about it. The research and articles used as proof of important concepts are readily accessible on the internet.
HEROIN- WHAT IS IT?
Heroin is diacetylmorphine. Once in the body, it rapidly breaks down into 6-mono-acetylmorphine, then morphine. After heroin was given intravenously in a clinical study, maximum concentration of morphine was reached in 7.8 minutes (I.V. avg.). (1) Heroin is considered a pro-drug for morphine, meaning it acts as a delivery system for morphine.
Morphine is a non-toxic central nervous system depressant drug that has two hallmark side effects: nausea and constipation. It is used predominately as an analgesic (pain reliever) and is considered the 'gold standard' in this field.
Therefore, heroin is not an inherently dangerous drug: it is nothing more than a way of administering morphine. Heroin is taken recreationally because of the euphoria and sense of well-being it can give due to its primary active metabolite, morphine. It can be inhaled (smoked), snorted, ingested, administered rectally/vaginally or injected.
DEFINITION OF OVERDOSE
“An excessive dose of a drug or substance” *
An overdose is an excessive dose of one drug or substance that leads to an adverse event directly attributable to that drug or substance. Regarding psychoactive substance use (and particularly central nervous system depressant drugs), an adverse event caused by the ingestion of two or more different classes of drugs cannot be correctly described as an overdose. The correct terminology is multiple or mixed-drug toxicity.
* Mosby's dictionary of medicine, nursing and health professions (2006)
SO-CALLED 'HEROIN OVERDOSE'
'Heroin overdose' is a term often used in relation to the death of a person who had heroin metabolites (predominately morphine) in their body. The clear inference is that taking 'too much' heroin resulted in death from 'respiratory depression' or arrest. In other words, the person is alleged or believed to have died as a result of their breathing having slowed markedly or actually stopping due to the effects of morphine. This concept has entered common folklore and is generally accepted without question in the general populace.
However, there is no evidence to even suggest that fatal 'heroin overdose' occurs. Furthermore, indisputable evidence demonstrates that it is a fallacy.
SUBSTANTIAL OVERDOSE CLINICALLY PROVEN NOT TO BE DANGEROUS
Amounts of heroin constituting 150% of the regular dose given to subjects receiving high-dose heroin maintenance therapy under clinical, controlled conditions, "...did not cause any serious side effect." (1) Moreover, "[c]hanges in heart rate, systolic and diastolic blood pressure, and skin temperature were marginal, less than 5%." The largest overdose administered was 150mg (450mg single I.V. dose for person on 300mg maintenance dose). This means the person was given 150mg more than they were accustomed to.
Subjects were also on methadone therapy, on which no dose limitations were set. The methadone was given two hours after the morning heroin dose. It is clear therefore, that amounts of heroin significantly more than the user is accustomed to are not dangerous.
LOW MORPHINE LEVELS
As regards people who have died with heroin metabolites present, it is consistently found that blood-morphine levels are low and in the range found in living people. The median blood-morphine level in an Australian study was 0.24 mg/L, which is an extremely low, therapeutic level. (4) This clearly indicates that the people did not die as a result of 'too much' heroin.
In a clinically demonstrated example, participants in research were given doses 67%, 100% and 150% of their regular maintenance doses of heroin. (1) The maximum morphine concentration in the subjects that received overdoses (maximum single I.V. heroin dose of 450mg) was 1.35 milligrams per litre of blood. (1:t2,p90) This is a level of morphine consistent with that found in people receiving morphine for pain.
It is clear that there is no evidential basis for problematic blood-morphine levels due to heroin overdose. Clinical research demonstrates low, non-problematic blood-morphine levels even after administration of extremely large amounts of heroin and in significant overdose.
THE METABOLISM OF MORPHINE
As the aforementioned study (1) demonstrated, an extremely large amount of heroin (450mg) introduced intravenously and rapidly as a single dose resulted in a low, therapeutic blood-morphine level not exceeding 1.35 mg/L. The human body has an extraordinary capacity for metabolising morphine and this explains why only very low levels are found in the 'recreational' context, where doses of heroin are typically a fraction of 450mg.
THERAPEUTIC MORPHINE LEVELS
Blood levels of morphine in a study involving patients with terminal, advanced cancer ranged from 0.010 mg/L (35 nmol/l) to 20 mg/L (70,302.6 nmol/l), with an average level of 1.6 mg/L (5617.8 nmol/l). (2:t2,p4) The levels of morphine in cases of deaths where heroin metabolites are found are almost exclusively a fraction of the average level in the patients described here, who were receiving morphine for pain.
NO MAXIMUM DOSE
'Maximum dose' is the level that when exceeded, can result in danger to the patient. As stated in 'Fundamentals of Nursing, Human Health and Function': "[t]here is no ceiling effect or maximum dose for opiate agonist drugs." (3) When used for analgesia (pain relief), morphine can be given until pain relief is achieved without regard to the size of the total dose: “[d]oses as large as 1654 mg IV morphine per hour (37,536 mg/day) have been administered."
This is indicative of three things. Firstly, morphine not being a drug proficient in compromising breathing to a dangerous degree. Secondly, the benign nature of the substance in terms of toxicity to the human body and thirdly, the rate at which the substance is metabolised.
'TOLERANCE'
Lack of 'tolerance' cannot be claimed to be a contributor to alleged opioid-related death from two perspectives:
 Zador et al. found: “...heroin-related deaths occurred overwhelmingly in people
who were male, of an avg. age of 30 years, and frequent users.” (4) Consistently, the vast majority of those
found to have died with heroin metabolites present were frequent users and therefore can be expected to have had some degree of 'tolerance' to
opioids. If lack of 'tolerance' was a fatal overdose risk-factor, opioid-naïve people could be expected to be well represented in statistics. They
are not.
Zador et al. found: “...heroin-related deaths occurred overwhelmingly in people
who were male, of an avg. age of 30 years, and frequent users.” (4) Consistently, the vast majority of those
found to have died with heroin metabolites present were frequent users and therefore can be expected to have had some degree of 'tolerance' to
opioids. If lack of 'tolerance' was a fatal overdose risk-factor, opioid-naïve people could be expected to be well represented in statistics. They
are not.
 The levels of morphine found in deaths where heroin metabolites have been detected
are only ever very low. The low levels found are not dangerous as regards the physiological effects of morphine. As previously noted, a large,
single, intravenous dose of heroin (450mg) results in a low, non-problematic level of morphine in blood. This indicates that the concept
of 'tolerance' is of little or no relevance as regards adverse events in which opioids are present.
The levels of morphine found in deaths where heroin metabolites have been detected
are only ever very low. The low levels found are not dangerous as regards the physiological effects of morphine. As previously noted, a large,
single, intravenous dose of heroin (450mg) results in a low, non-problematic level of morphine in blood. This indicates that the concept
of 'tolerance' is of little or no relevance as regards adverse events in which opioids are present.
IMPURITIES
Studies have shown little evidence of dangerous impurities: “...studies of both NSW heroin seizures and heroin-related fatalities have shown the presence of dangerous adulterants such as quinine to be rare. Heroin in NSW is typically “cut” with inert substances such as sucrose and caffeine.” (6)
INARGUABLE PROOF THAT FATAL 'HEROIN OVERDOSE' DOES NOT EXIST
 Substantial, unexpected overdoses of heroin
(150%) given to people on high-dose maintenance treatment in clinical, controlled conditions, proven to be of no concern.
Doses of 150mg more than the person's usual maintenance dose "...did not cause any serious side effect." (1)
Substantial, unexpected overdoses of heroin
(150%) given to people on high-dose maintenance treatment in clinical, controlled conditions, proven to be of no concern.
Doses of 150mg more than the person's usual maintenance dose "...did not cause any serious side effect." (1)
Accordingly, from the perspective of overdose, it is clear that heroin is not dangerous.
 Single intravenous doses of up to 450mg of heroin under
clinical, controlled conditions, result in low, non-problematic blood-morphine levels. A maximum blood-morphine level of 1.35 mg/L
occurs during the study. (1)
Single intravenous doses of up to 450mg of heroin under
clinical, controlled conditions, result in low, non-problematic blood-morphine levels. A maximum blood-morphine level of 1.35 mg/L
occurs during the study. (1)
Accordingly, from the perspective of blood-morphine levels, it is clear that morphine from the 'recreational' use of heroin or morphine, does not reach dangerous levels in the blood.
MULTIPLE-DRUG TOXICITY
Multiple-drug toxicity is in effect, profound and disabling sedation caused by the presence of multiple classes of central nervous system depressant drugs. The consequence of combining drugs can be a sedating effect far in excess of that caused by either drug taken by itself. This heavy sedation can lead to airway obstruction and resultant breathing difficulties. Breathing can become restricted or impossible, which can lead to hypoxic brain damage and ultimately, death.
A combination of alcohol and morphine for instance, can be dangerous. An Australian study found 45% of a sample of deaths where heroin metabolites were detected also had alcohol present, with an average blood-alcohol level of 0.14 g/100ml. (4) Benzodiazepines were found in 26% of cases. The study noted that: “[i]n 71% [of subjects], two or more different drugs were found at autopsy...”.
The study also noted that: “[a]lthough alcohol was detected in 45% of subjects at time of death, it was noted on the death certificate in only 7% of cases.”
DEATHS OR ADVERSE EVENTS INCORRECTLY ATTRIBUTED TO 'HEROIN OVERDOSE' ARE ACTUALLY CAUSED BY:
1. ASPHYXIATION (deficient supply of oxygen) due to airway obstruction. This is a result of heavy sedation caused by ingestion of multiple substances (not heroin alone). When a person is heavily sedated, they can lose the ability to keep their airway open and as a result, they cannot breathe properly. This can lead to injury or death due to lack of oxygen.
2. UNKNOWN CAUSES (non drug-related), with low levels of heroin metabolites (predominately morphine) found.
EXAMPLE OF INCORRECT USE OF THE TERM 'HEROIN OVERDOSE'
A study examining heroin use in an Australian city defined 'heroin overdose' as: “...where a positive response to ... Naloxone (Narcan) has been observed for those people unconscious at time of initial ambulance attendance...”. (7)
1. This definition does not take into account the presence of other drugs. Use of the term 'heroin overdose' to describe a situation of problematic sedation without considering or testing for the presence of drugs other than opioids, is not valid.
2. Heroin use is established by the presence of 6-monoacetylmorphine by toxicological analysis. A positive response to naloxone (a drug that reverses the effects of opioids) merely suggests the presence of an opioid: it cannot specifically implicate heroin.
CORONERS / FORENSIC PATHOLOGISTS
There is a long history of attributing cause of death solely to heroin regardless of the presence of other drugs and/or low morphine levels and when no definitive cause can be identified. The following, by a forensic pathologist, illustrates this:
“The general approach seems to be that scene evidence of illicit intravenous drug use, plus a history of recurrent heroin use, an essentially negative autopsy and detection of heroin metabolites (ie morphine) in blood is sufficient for attributing death to the administration of heroin. This is despite the fact that low therapeutic levels of morphine may be detected, or that significant quantities of other drugs may be found in blood, typically alcohol and benzodiazepines.”
“Toxicological findings in apparently obvious heroin overdose deaths are puzzling, with generally low morphine levels detected in blood…”
"…it is highly unusual to find levels of morphine in illicit intravenous heroin users in the range seen in palliative care patients."
"…this has resulted in forensic pathologists using a variety of terms to circumvent the obvious fact that an overdose in the classical sense of the word did not take place."
All quotes Duflou (5)
EXAMPLES OF INACCURATE CLASSIFICATION AND REPORTING
Following are two examples of multiple-drug toxicity deaths in which incorrect statements were made regarding the cause of death:
1. Janis Joplin (singer) died in 1970. The cause of death was officially recorded as: “[a]cute heroin-morphine intoxication due to: injection of overdose.” (8) The toxicology report noted a substantial blood-alcohol level with a low blood-morphine level: “[b]lood: Ethanol (alcohol) .11 percent, Blood: Morphine 0.02 mg. percent.”
It was inaccurate to classify her death as resulting from an opioid overdose, as alcohol was also present. The case is a typical example of a multiple-drug toxicity event involving an extremely low morphine level and a substantial level of alcohol.
2. Ms 'A' died in Melbourne, Australia in 2016. Her death received widespread media coverage as resulting from 'heroin overdose'. In the coroner's report, the following was stated: "[m]s A fatally overdosed on heroin." (9:p7)
However, Ms A's death was not caused by 'heroin overdose':
 There was no evidence that heroin was used. The indicator of heroin use,
6-monoacetylmorphine, was not detected.
There was no evidence that heroin was used. The indicator of heroin use,
6-monoacetylmorphine, was not detected.
 The level of morphine found was very low: 0.3 mg per litre of blood
The level of morphine found was very low: 0.3 mg per litre of blood
 Multiple substances were detected. As well as morphine and codeine,
nitrazepam (0.03 mg/L, a benzodiazepine) and diphenhydramine (0.07 mg/L, an anti-histamine) were found. (9:p4)
Multiple substances were detected. As well as morphine and codeine,
nitrazepam (0.03 mg/L, a benzodiazepine) and diphenhydramine (0.07 mg/L, an anti-histamine) were found. (9:p4)
Ms A's medical cause of death was originally classified as "...GLOBAL CEREBRAL ISCHAEMIA SECONDARY TO PROBABLE HEROIN TOXICITY." It was subsequently amended to "...GLOBAL CEREBRAL ISCHAEMIA SECONDARY TO MIXED DRUG TOXICITY INCLUDING A SUBSTANCE CONSISTENT WITH HEROIN." (9:p5)
Use of the term 'overdose' or 'heroin overdose' in describing this death is not valid in any way. The case is a typical example of a multiple-drug toxicity event involving an extremely low morphine level and the presence of other substances. The probable cause of Ms A's death was asphyxiation due to airway obstruction in the context of heavy sedation.
HEALTH EFFECTS
Apart from nausea and constipation, hazards associated with use are largely due to the illegal nature of heroin possession and supply. Given a legal and pure supply, heroin can be used with relative safety. The most serious problem with long-term opioid use is constipation (if not managed effectively). Chronic constipation is not a desirable circumstance from the perspective of general health.
DEPENDENCE / ADDICTION
If enough heroin is taken for long enough, physical dependence to morphine will occur. The withdrawal syndrome initiated by sudden abstinence is commonly likened to a 'bad case of the flu'. Morphine withdrawal is not regarded as life-threatening.
Heroin is not 'instantly addictive'; the vast majority of people that try heroin have a distinctly unpleasant experience due to nausea and are therefore discouraged from taking the substance again.
An extremely low percentage of the total population regularly take opioids on a 'recreational' basis due to their unpleasant side effects: nausea and constipation. Very few people are prepared to tolerate these side effects in order to consistently use the substances.
CONCLUSION
HEROIN:
 IS NOT TOXIC. Heroin (morphine) nauseates and constipates.
IS NOT TOXIC. Heroin (morphine) nauseates and constipates.
 IS PROVEN NOT TO BE DANGEROUS IN SUBSTANTIAL OVERDOSE
IS PROVEN NOT TO BE DANGEROUS IN SUBSTANTIAL OVERDOSE
It is not 'deadly' or 'dangerous' and does not 'kill people'. It is merely a delivery system for morphine. When heroin is involved in drug-related adverse events related to breathing, it is as part of a combination with other 'depressant' drugs. A combination of central nervous system depressant drugs is known to be potentially dangerous due to heavy sedation leading to airway obstruction and subsequent breathing difficulties.
SUPERVISED INJECTING FACILITIES AND NALOXONE
SUPERVISED INJECTING FACILITIES
So-called 'supervised' or 'safe' injecting facilities, where people can use substances intravenously with medical support and clean injecting equipment can be a useful service for injecting-drug users. However, some points must be made to counter the myths surrounding them:
 Most importantly, these facilities do not 'save' people from 'heroin overdose'. They
have the ability to assist those affected by multiple-drug toxicity: people who succumb to heavy sedation from mixing drugs and are in danger of
airway obstruction.
Most importantly, these facilities do not 'save' people from 'heroin overdose'. They
have the ability to assist those affected by multiple-drug toxicity: people who succumb to heavy sedation from mixing drugs and are in danger of
airway obstruction.
 Such facilities are not necessary for people to safely use heroin intravenously.
People who have clean injecting equipment, a pharmaceutical-grade supply of heroin and who do not mix drugs have no need for such a facility,
although they may choose to use one.
Such facilities are not necessary for people to safely use heroin intravenously.
People who have clean injecting equipment, a pharmaceutical-grade supply of heroin and who do not mix drugs have no need for such a facility,
although they may choose to use one.
 The term 'safe' or 'supervised' injecting facility implies that the only way heroin
can be used safely (intravenously or otherwise) is in one of these facilities. This of course, is not true. The facilities are promoted by
governments and those financially sustained by them as a necessary intervention to prevent death and adverse events due to
'heroin overdose': a portrayal that is totally incorrect and intentionally misleading.
The term 'safe' or 'supervised' injecting facility implies that the only way heroin
can be used safely (intravenously or otherwise) is in one of these facilities. This of course, is not true. The facilities are promoted by
governments and those financially sustained by them as a necessary intervention to prevent death and adverse events due to
'heroin overdose': a portrayal that is totally incorrect and intentionally misleading.
The fundamental, ethical and sensible interventions for the current situation of opioid users having the supply and possession of their drug of choice subject to criminal sanctions, are as follows:
 Having the possession of opioids not subject to criminal sanctions,
as is the case with the possession of alcohol, tobacco and caffeine
Having the possession of opioids not subject to criminal sanctions,
as is the case with the possession of alcohol, tobacco and caffeine
 Providing opioid users with a legal and regulated supply of their
drug of choice, as is the case with the supply of alcohol, tobacco, and caffeine
Providing opioid users with a legal and regulated supply of their
drug of choice, as is the case with the supply of alcohol, tobacco, and caffeine
 Governments ceasing to promote the myth of fatal 'heroin overdose'
and instead informing of the true hazard, which is the combining of different classes of central nervous system depressant drugs
Governments ceasing to promote the myth of fatal 'heroin overdose'
and instead informing of the true hazard, which is the combining of different classes of central nervous system depressant drugs
NALOXONE (NARCAN)
Naloxone is a drug that 'reverses' the effects of opioids. It displaces (removes) opioids from opioid receptors in the brain and attaches to the receptor in place of the opioid, but does not exert an effect. Therefore, if administered to an opioid-dependent person, it can initiate a withdrawal syndrome.
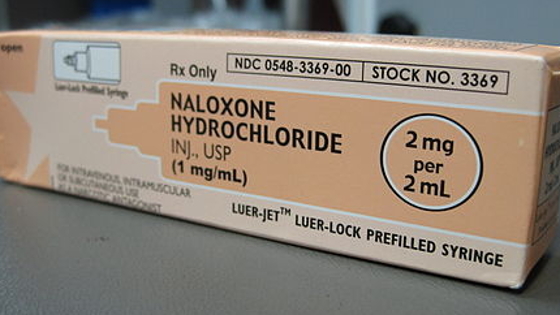
Image: Intropin
Similar to 'supervised injecting facilities', naloxone can be the subject of incorrect assertions regarding its use and capabilities:
 Naloxone does not 'save' people from alleged potentially fatal 'opioid overdose'.
It can remove the opioid component of dangerous sedation caused by multiple classes of central nervous system depressant drugs. This sedation can
lead to airway obstruction and possible asphyxiation.
Naloxone does not 'save' people from alleged potentially fatal 'opioid overdose'.
It can remove the opioid component of dangerous sedation caused by multiple classes of central nervous system depressant drugs. This sedation can
lead to airway obstruction and possible asphyxiation.
 The immediate and necessary intervention for a person affected by dangerous
sedation caused by multiple classes of central nervous system depressant drugs, is airway monitoring and if necessary, support. The airway must
be confirmed as open before other interventions are considered.
The immediate and necessary intervention for a person affected by dangerous
sedation caused by multiple classes of central nervous system depressant drugs, is airway monitoring and if necessary, support. The airway must
be confirmed as open before other interventions are considered.
 Naloxone is being aggressively promoted as the antidote for alleged potentially
fatal 'opioid overdose'. This is wholly misleading and dangerously incorrect. Firstly, fatal 'opioid overdose' does not exist: the danger is
mixing drugs. Naloxone is being portrayed as the solution to a phenomenon that does not exist, whilst the true danger is being largely ignored.
Naloxone is being aggressively promoted as the antidote for alleged potentially
fatal 'opioid overdose'. This is wholly misleading and dangerously incorrect. Firstly, fatal 'opioid overdose' does not exist: the danger is
mixing drugs. Naloxone is being portrayed as the solution to a phenomenon that does not exist, whilst the true danger is being largely ignored.
Secondly, the loss of consciousness caused by mixed-drug toxicity can occur rapidly. The absolute priority is securing the affected person's airway before oxygen deprivation can occur. The administration of naloxone is secondary to ensuring an open airway.
Naloxone is of no assistance to a solitary person who is unconscious due to multiple-drug toxicity, as they are unable to self-administer the substance. The only truly effective strategy in terms of avoiding harm due to multiple-drug toxicity is the avoidance of drug combinations.
The provision of naloxone as the panacea to 'opioid overdose' presents a significant commercial opportunity. This opportunity however, is at the expense of the truth and ultimately the welfare of those whose drug of choice happens to be opioids.
REFERENCES
1. Pharmacokinetics and pharmacodynamics of high doses of pharmaceutically prepared heroin, by intravenous or by inhalation route in opioid-dependent patients. Elisabeth J. Rook et al. From Basic and Clinical Pharmacology and Toxicology, 98, 86-96. (2006)
2. Serum and urine concentrations of morphine and morphine metabolites in patients with advanced cancer receiving continuous intravenous morphine: an observational study. Lee, Yong Joo et.al. BMC Palliative Care. (2015)
3. Fundamentals of Nursing, Human Health and Function. Craven, Hirnle. 5th ed., page 1201. (2007)
4. Heroin-related deaths in New South Wales, 1992: toxicological findings and circumstances. Zador, Sunjic and Darke. (1997)
5. Classification of opioid deaths – a forensic pathologist’s perspective. Johan Duflou, NSW Institute of Forensic Medicine. (N.D.)
6. NSW DRUG TRENDS 2000, Findings from the Illicit Drug Reporting System (IDRS). Shane Darke, Libby Topp & Sharlene Kaye. NDARC Technical Report No. 117.
7. Heroin use in Geelong, an investigation into the impact of heroin use on a major regional centre. Peter Miller. School of Social Inquiry, Deakin University. (2000)
8. Copies of original coronial and police documents from www.autopsyfiles.org.
9. Finding into death with inquest. Findings of Coroner Jacqui Hawkins on death of 'Ms A'. Coroner's Court of Victoria (Australia) document. Court Reference: COR 2016-2418. (2017)
RECOMMENDED READING
Chapter 12. The "heroin overdose" mystery and other occupational hazards of addiction. The Consumers Union Report on Licit and Illicit Drugs. Edward M. Brecher and the Editors of Consumer Reports Magazine. (1972)
Page head image: Antique heroin bottle by Oxfordian Kissuth (cropped). Lic.- Creative Commons Attribution - Share Alike 3.0 Unported
